
Contrary to the mistaken belief that hair loss primarily afflicts males, it might be surprising to learn that women constitute forty percent of hair loss sufferers. The consequences of hair loss for women extend well beyond the physical aspects, significantly impacting their self-image and emotional well-being.
Tragically, societal norms have effectively silenced women, compelling them to bear their struggles quietly, while the medical community largely disregards the issue of women’s hair loss.
Introduction
Mainstream medicine, including general practitioners, gynecologists, and dermatologists, often lacks the specialized expertise needed to effectively diagnose and treat the different forms of hair loss that affect women. Additionally, many physicians exhibit a lack of compassion and empathy towards women experiencing hair loss, exacerbating their feelings of hopelessness and disheartenment. As a result, many patients are left feeling marginalized and invalidated due to the insufficient support and dismissive responses they receive.
Contrary to the perception that hair loss is not life-threatening, the psychological repercussions of feeling unattractive and experiencing hair loss can be just as devastating as any severe disease, taking a toll on both mental and physical health. The impact on women goes far deeper than simply feeling less attractive; it is profound and touches the very core of their being.
The American Hair Loss Association recognizes that hair loss is a woman is a serious life altering
condition that can no longer be ignored by the medical community and society as a whole.
For many women, hair loss can lead to a profound sense of loss and can cause them to question their identity, femininity, and overall sense of
self. Hair has long been associated with beauty and femininity, and its loss can leave women feeling disconnected from their own sense of womanhood.
It can shatter their confidence and undermine their self-esteem, affecting every aspect of their lives, from personal relationships
to professional endeavors.
The emotional distress caused by hair loss can lead to social withdrawal, anxiety, and clinical depression.
Women may find themselves avoiding social situations and isolating themselves, fearing judgment and ridicule.
They might struggle to participate in activities they once enjoyed, leading to a further decline in their overall well-being.
The quest to conceal or cope with hair loss can become an all-consuming focus for many women, impacting their daily lives and routines.
Female Pattern Hair Loss (Androgenetic Alopecia):

Genetic female pattern hair loss, long believed to be analogous to male pattern baldness with only slight differences in presentation, manifests as diffuse hair thinning across the entire scalp, while typically retaining some degree of the frontal hairline. Initially, it was widely believed that androgen hormones, similar to male pattern baldness, played a major role in driving this condition. However, current understanding reveals that androgenetic hair loss in women is not solely dictated by male hormones.
Contrary to the previous assumption, most women with Androgenetic Alopecia actually have normal hormone levels, except in cases where they are taking exogenous hormones, notably hormonal birth control. Remarkably, about 90% of women affected by Androgenetic Alopecia show normal naturally occurring (androgen) levels. Interestingly, despite the normal or low-normal hormone levels, treatments specifically targeting androgens for Androgenetic Alopecia can still prove effective.
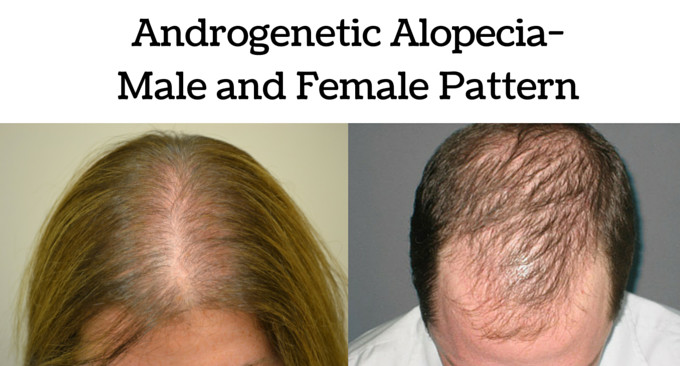
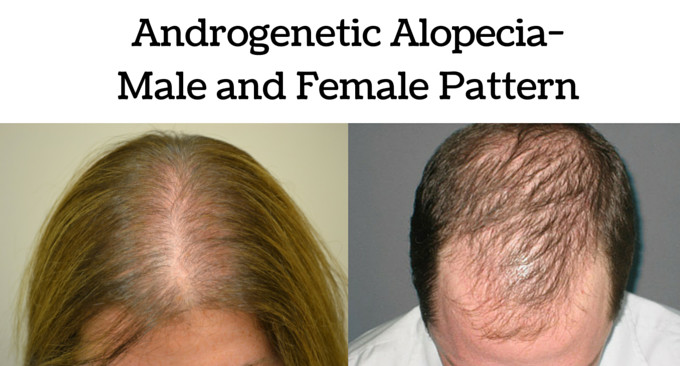
Differences between Female Pattern Hair Loss (FPHL) and Male Pattern Hair Loss:
Female pattern hair loss (FPHL) is characterized by diffuse hair thinning throughout the entire scalp, often retaining some degree of the frontal hairline. Unlike male pattern baldness, androgens have a less clear-cut role in FPHL, and blocking these hormones may not always be beneficial. In fact, increasing androgen hormones may help some women.
The genetics of hair loss in women are more complex, and some women experience genetic hair loss without a strong family history of the condition.
Alterations in estrogen signaling may play an important role in FPHL.
In women with FPHL, the efficacy of the drug finasteride (commonly used to treat hair loss in men) cannot be predicted with the same degree of certainty as in men with androgenetic alopecia (AGA).
The patterns of hair loss differ, with women experiencing central scalp hair loss (generally) while men lose hair in the temples and crown of the head.
Am extremely small percentage (less than 5%) of women are suitable candidates for hair transplant surgery due to the impact of genetic hair loss on the donor area.
Females have significantly lower levels of 5 alpha reductase compared to men.
Women have higher aromatase levels, which convert testosterone to estradiol and estrone, reducing the conversion to dihydrotestosterone (DHT). Aromatase levels are particularly elevated in the frontal hairlines of women compared to men. These differences may explain why retention of the frontal hairline is a typical feature of FPHL but not observed in male balding.
Although androgen receptor levels are higher in the frontal scalp than the occipital scalp in both men and women, the total receptor level is 40% lower in women.
Types of Hair Loss:
The word “alopecia” is the medical term for hair loss. Alopecia does not refer to one specific hair loss disease — any form of hair loss is alopecia. The word alopecia is Latin, but can be traced to the Greek “alopekia,” which itself comes from alopek, meaning “fox.” Literally translated, the word alopecia (alopekia) is the term for mange in foxes. Hair loss can be caused by any number of conditions, reflected in a specific diagnosis. Some diagnoses have alopecia in their title, such as alopecia areata or scarring alopecia, but many do not, such as telogen effluvium.
Alopecia can be caused by many factors from genetics to the environment. While androgenetic alopecia (male or female pattern baldness, AGA for short) is by far the most common form of hair loss, dermatologists also see many people with other forms of alopecia. Several hundred diseases have hair loss as a primary symptom.
Among the most frequent non-AGA alopecias seen by dermatologists are telogen effluvium, alopecia areata, ringworm, scarring alopecia, and hair loss due to excessive cosmetic treatment. Less common types of hair loss might pose diagnostic challenges, leading patients to wait for months, or even years, seeking consultations with multiple dermatologists until they find one knowledgeable about their condition. Moreover, for rare diseases, research motivation might be limited, hindering the development of treatments. Often, even after a correct diagnosis, dermatologists might have no known treatment to offer for the condition.
Androgenetic Alopecia:
Androgenetic alopecia, commonly known as male or female pattern baldness, is the most prevalent form of hair loss affecting both genders. This condition is characterized by a progressive thinning of hair, following a distinct pattern on the scalp.
Men typically experience a receding hairline combined with thinning at the crown, which can lead to complete baldness. In contrast, women usually observe a diffuse thinning across the scalp, with the frontal hairline often remaining intact but thinned.
The development of androgenetic alopecia results from a complex interplay of genetic predisposition, hormonal factors, age, and recently identified inflammatory processes.
Genetic and Hormonal Underpinnings:
The genesis of androgenetic alopecia is rooted in genetic factors that predispose individuals to the condition, affecting how their hair follicles respond to dihydrotestosterone (DHT), a potent derivative of testosterone. The enzyme 5-alpha reductase is solely responsible for converting testosterone into DHT. Its critical role is in facilitating this conversion, thereby increasing the levels of DHT available to interact with androgen receptors on the hair follicles. This interaction between DHT and the follicle’s androgen receptors, influenced by genetic predisposition, leads to a shortened hair growth cycle and the miniaturization of follicles, resulting in hair thinning and loss.
Individuals with androgenetic alopecia have hair follicles that are genetically programmed to be sensitive to DHT. This sensitivity triggers a series of cellular responses that lead to the follicle’s shrinkage and a diminished capacity to produce healthy, thick hair. The role of hormones, particularly DHT, is crucial as it directly influences the hair growth cycle, progressively leading to the characteristic patterns of hair loss seen in androgenetic alopecia.
The Inflammatory Component:
Recent research has unveiled an inflammatory component that significantly contributes to the severity and progression of androgenetic alopecia. This aspect involves the activation of immune cells around the hair follicles, leading to the release of cytokines and other inflammatory mediators. Such inflammatory processes not only exacerbate follicular miniaturization but also can lead to fibrosis, making the condition more severe and potentially accelerating the transition to irreversible hair loss.
Age-Related Factors and Implications for Treatment:
The onset and progression of androgenetic alopecia are significantly influenced by age. Men may start noticing signs as early as their late teens or early twenties, with the risk of hair loss increasing as they age. For women, significant thinning typically occurs post-menopause, when hormonal shifts can amplify DHT’s detrimental effects on hair follicles. However, early-onset female pattern baldness has become more prevalent in recent decades. This trend is partly attributed to the earlier use of hormonal contraception among young women, which artificially induces hormonal changes that can trigger androgenetic alopecia (AGA) decades earlier than it might have occurred naturally. Furthermore, more than half of women today begin experiencing AGA much earlier than previous generations, marking a significant shift in the age-related patterns of this condition.
Understanding the multifaceted nature of androgenetic alopecia, especially the roles of DHT and the inflammatory response, has been pivotal in developing treatments. Therapies targeting the reduction of DHT levels, such as finasteride and dutasteride, have shown tremendous efficacy. Moreover, emerging treatments aiming to mitigate scalp inflammation offer a promising avenue for more comprehensive management strategies.
Conclusion:
Androgenetic alopecia is a complex condition that goes beyond simple genetic predisposition, encompassing hormonal, inflammatory, and age-related factors. The interplay between DHT sensitivity, enzyme activity, and inflammation underscores the need for a multifaceted therapeutic approach. As research continues to evolve, understanding these underlying mechanisms will be key to devising more effective treatments, offering hope to millions affected by the most prevalent form of hair loss.
Effluviums:
Certain hair loss conditions are known as “effluviums,” a term denoting an outflow. Effluviums specifically impact various phases of the hair growth cycle. Hair follicles on the scalp don’t maintain a continuous production of hair. Instead, they cycle through a growth phase that can extend for two or more years, followed by a resting stage lasting up to two months before initiating the growth of a new hair fiber. At any given time on a healthy human scalp, approximately 80% to 90% of the hair follicles are actively growing hair. These active follicles are in what’s known as the anagen phase. This leaves around 10% to 20% of scalp hair follicles in a resting state called telogen, during which they don’t produce any hair fiber.
Telogen Effluvium:
Telogen effluvium (TE) is likely the second most common type of hair loss encountered by dermatologists.
It remains a vaguely defined condition, with minimal research conducted to fully understand TE. Essentially,
TE occurs when there is a shift in the number of hair follicles that are actively growing hair.
If the count of hair follicles producing hair significantly drops, particularly during the resting (telogen) phase,
there’s a notable increase in dormant telogen-stage hair follicles. This results in shedding, or TE hair loss.

TE appears as a diffuse thinning of hair across the scalp, which may not be evenly distributed. It can be more pronounced in certain areas of the scalp. Typically, hair thinning is more evident on the top of the scalp compared to the sides and back. Hairline recession is generally absent, except in rare chronic cases.
The hairs shed in TE are typically telogen hairs, recognizable by a small bulb of keratin at the root end. Whether this keratinized mass is pigmented or not doesn’t affect the classification; these hair fibers remain typical telogen hairs.
Individuals with TE usually don’t experience complete scalp hair loss, but in severe cases, noticeable hair thinning can occur. While TE is typically localized to the scalp, more severe instances can affect other areas, such as the eyebrows or pubic region. Regardless of the form TE takes, it is completely reversible. The hair follicles aren’t permanently or irreversibly damaged; they simply enter a resting state in larger numbers than normal.
TE can develop in three primary ways:
ENVIRONMENTAL SHOCK: An abrupt environmental shock can trigger hair follicles to enter a resting state temporarily. This results in increased hair shedding and diffuse thinning of hair on the scalp. This form of TE can develop rapidly and might become noticeable one or two months after the triggering event. If the trigger is short-lived, the hair follicles will return to their growing state and start producing new hair fibers relatively quickly. This type of TE usually lasts less than six months, and affected individuals typically regain normal scalp hair density within a year.
GRADUAL ACCUMULATION: Hair follicles might transition more slowly to a resting telogen state and remain there for an extended period, leading to a gradual accumulation of telogen-stage follicles and progressive thinning of scalp hair. There might not be substantial hair shedding, but gradual thinning occurs. This form of TE is more likely in response to a persistent trigger.
TRUNCATED GROWTH CYCLES:
In this type of TE, hair follicles don’t stay in a resting state but rather cycle through shortened growth stages.
This results in thin scalp hair and persistent shedding of short, thin hair fibers.
Causes of Telogen Effluvium: Stress and Diet
Numerous factors can trigger TE. Short-term TE often occurs in women shortly after childbirth, referred to as postpartum alopecia. The sudden hormonal change during childbirth can shock hair follicles into a temporary resting state, causing significant hair shedding. However, most women quickly regrow their hair after this phase.
Similarly, vaccinations, crash diets, physical trauma (such as a car crash), and surgeries can temporarily send a proportion of scalp hair follicles into hibernation. As the body recovers from these shocks, TE subsides, and new hair growth resumes.
Certain drugs, especially antidepressants, can also induce TE. Switching to a different medication might resolve this issue.
More persistent insults can lead to prolonged TE. For example, chronic illnesses can result in TE. Chronic stress and dietary deficiency are arguably the two most common triggers. Many dermatologists believe chronic stress gradually exerts a negative impact on hair growth, leading to persistent TE. Research with animal models supports this claim, indicating a connection between stress, changes in hair follicle biochemistry, and an increased number of hair follicles entering the telogen resting state.
Debates among dermatologists surround the role of dietary problems in causing TE in North America. While dietary deficiencies can certainly cause TE, particularly in third-world countries where diets may lack essential nutrients, it’s a contentious topic in developed nations. In first-world countries, the average diet is rarely entirely deficient in a particular vitamin or mineral. However, some dermatologists argue that reduced red meat consumption and a preference for vegetarian diets might result in imbalanced nutrient intake, particularly regarding iron deficiency in women due to regular iron loss during menstruation.
Other potential deficiencies in the modern North American diet, such as insufficient zinc, amino acid L-lysine, or vitamins B6 and B12, have also been proposed as contributors to TE.
When dietary deficiencies are suspected, supplements might be recommended. However, supplements can pose issues. Our bodies can only process a limited amount of iron each day, and high doses of iron can be toxic and lead to hair loss. Excessive vitamin A from supplements can also trigger TE reactions in some individuals, as excessive vitamin A can be toxic.
TE can occur independently or alongside other diseases. The early stages of androgenetic alopecia (male or female pattern baldness, AGA for short) are effectively TE. Early AGA is marked by an increase in resting telogen hair follicles, with up to 40% of scalp hair follicles in telogen phase.
TE can also manifest as a symptom of other conditions, such as inflammatory conditions like alopecia areata. Hair follicles are sensitive to thyroid hormones, and about one-third of individuals with thyroid disorders experience TE. Exposure to toxins can also cause TE as part of a broader set of symptoms.
Before concluding the discussion on TE, it’s important to note that natural hair shedding is a normal process.
Seasonal variations in hair shedding have been observed, with more hair loss occurring in the fall and to a lesser extent in the spring. This temporary increase in telogen hair follicles and shedding might be attributed to hormonal fluctuations in response to changes in daylight exposure.
Anagen Effluvium:
Anagen effluvium mirrors telogen effluvium’s diffuse hair loss but develops much more rapidly and can lead to complete hair loss. This condition often arises in people taking cytostatic drugs for cancer treatment or those exposed to toxic substances like rat poison.
These substances inhibit rapid cell proliferation, a desirable effect for halting cancer cell growth. However, hair follicle cells are among the body’s fastest-growing noncancerous cells. Hair fibers from scalp hair follicles can grow at a rate of up to 0.4mm per day, requiring substantial cell proliferation. Cytostatic cancer drugs and toxins inhibit rapid cell growth, including hair follicle cell proliferation. This sudden inhibition halts hair fiber production.
The onset of anagen effluvium is swift. Individuals taking anticancer drugs may experience clumps of hair falling out within the first two weeks. Unlike telogen effluvium, the follicles don’t enter a telogen resting state but essentially freeze in time. Hair fibers shed quickly, often appearing as dystrophic anagen hairs with a tapered or feathered root end.
The extent of hair loss due to cytostatic drugs varies. Some individuals might experience a combination of anagen effluvium and telogen effluvium, resulting in limited hair loss.
Cold therapy, involving the use of ice packs or a specialized hood filled with cold water during anticancer drug administration, is employed by some cancer treatment centers to mitigate hair loss. Cold therapy induces a suspended animation in hair follicles before contact with the drug, preventing follicle cell uptake and damage. However, concerns exist that this approach might also shield cancer cells in the skin from the drug.
Experimental drugs to prevent drug-induced hair loss are being explored, but the same concern applies – these treatments could potentially safeguard cancer cells in the skin.
While anagen effluvium develops rapidly, recovery is equally swift. The follicles remain intact and poised for growth once the triggering factor is removed. After completing anticancer drug treatment, new hair growth may become visible within a month. Since the follicles are unharmed, normal hair density is restored. However, changes in hair fiber characteristics might occur, such as transitioning from straight to curly or experiencing altered hair color. These changes can be permanent.
Scarring Alopecia (Cicatricial Alopecia):
Scarring alopecia, also known as cicatricial alopecia, refers to a group of hair loss disorders that may affect
up to 3% of individuals experiencing hair loss. It occurs worldwide, impacting otherwise healthy men and women of all ages.

While each specific diagnosis within this category is relatively uncommon,
notable examples include dissecting cellulitis, eosinophilicpustular folliculitis,
follicular degeneration syndrome (formerly referred to as “hot comb” alopecia), folliculitis decalvans, lichen planopilaris,
and pseudopelade of Brocq. Scarring alopecia can also be part of more comprehensive conditions like chronic lupus erythematosus, where various organs of the body may be involved.
Despite the diversity of scarring alopecia forms, the common underlying theme is the potential for permanent and irreversible
destruction of hair follicles, leading to their replacement with scar tissue.
Most cases of scarring alopecia initially manifest as small patches of hair loss that may gradually expand over time. While some instances of hair loss occur gradually and go unnoticed due to minimal symptoms, others are accompanied by intense itching, burning, and pain, progressing rapidly.
The appearance of scarring alopecia patches often differs from that of alopecia areata, with the edges of the bald patches appearing more irregular. The damage to the hair follicles occurs beneath the skin surface, often resulting in minimal visible changes on the scalp skin other than patchy hair loss. Affected areas may exhibit smoothness and cleanliness, or they could display signs of redness, scaling, pigmentation changes, or even raised blisters oozing fluids or pus.
While these visual cues can aid in diagnosis, identifying scarring alopecia based solely on hair loss patterns and scalp skin characteristics can be challenging. A definitive diagnosis often requires one or more skin biopsies to confirm the condition and specify the precise type of scarring alopecia. Typically, a small biopsy ranging from 2 to 4 mm in diameter is conducted and analyzed under a microscope. Dermatologists and pathologists examine the biopsy for indicators such as follicle destruction, deep scar tissue, and the presence and location of inflammation relative to hair follicles.
Men’s Hair Loss:
Androgenetic alopecia, also known as common male pattern baldness (MPB), is responsible for over 95% of hair loss in men. By the age of thirty-five, two-thirds of American men will experience some degree of noticeable hair loss, and by the age of fifty, approximately 85% of men will have significantly thinning hair. Around 25% of men with male pattern baldness begin losing hair before the age of twenty-one.
Introduction:
Contrary to popular belief, most men who suffer from male pattern baldness are extremely unhappy with their situation and would do anything to change it. Hair loss affects every aspect of a sufferer’s life, from interpersonal relationships to professional opportunities. In fact, the American Hair Loss Association (AHLA) has received countless reports from young men who felt so overwhelmed and distracted by their progressive hair loss that they were forced to change their career paths.
Recognizing the devastating impact of male pattern baldness on men of all ages, the AHLA has created resources to provide objective answers to hair loss questions. We strongly advise against relying on commercial websites and social media platforms for information, unless they carry the AHLA seal or the AHLA Trusted Content Creator distinction. Many products and services being sold online to vulnerable hair loss consumers are not backed by scientific evidence. Currently, only two FDA-approved products have been clinically proven to stop or prevent hair loss, and only a relative handful of surgeons are performing surgical hair restoration to state-of-the-art standards.
In addition to male pattern baldness, this section will also discuss other forms of alopecia that can affect a smaller subset of people. The AHLA is dedicated to providing comprehensive information and education to support men who are experiencing hair loss, empowering them to make informed decisions during their hair loss journey.
 Diagnosis:
Diagnosis:
Typical male pattern baldness is usually diagnosed based on the appearance and pattern of the hair loss, along with a detailed medical history, including questions about the prevalence of hair loss in your family. An experienced medical hair loss expert should examine the scalp under magnification (preferably with a device called a densitometer), in order to assess the degree of miniaturization of the hair follicles. This can help determine if the hair loss is consistent with male pattern baldness.
In some cases, if the physician suspects another form of alopecia or if the hair loss appears to have a diffuse pattern, they may suggest a scalp biopsy to confirm the diagnosis. Scalp biopsy involves taking a small sample of the scalp tissue for microscopic examination to determine the cause of hair loss. However, in general, the diagnosis of male pattern baldness is relatively straightforward based on the characteristic pattern of hair loss.
It’s important to note that some advertised “clinics” may recommend costly hair analysis or scalp biopsy as part of their diagnostic process, but these may not be necessary for typical male pattern baldness. The only reason to have a hair analysis is to assess the possibility of poison-induced hair loss, which is rare. Hair analysis may reveal substances such as arsenic or lead, but hair loss caused by poisoning does not typically present itself in a typical male pattern. It’s important to seek the advice of a qualified physician who can properly examine and diagnose your hair loss, and avoid unnecessary and costly tests or procedures.
Causes of Hair Loss:
Androgenic alopecia, commonly known as male pattern baldness (MPB), is the primary cause of hair loss in men, and it can be triggered anytime after puberty due to the genetic susceptibility to the effects of Dihydrotestosterone (DHT) which varies widely. While there can be various reasons for hair loss, such as serious illness, reaction to medications, or exceptionally stressful events, heredity is often to blame for most cases of hair loss in men. Despite the myth that baldness is solely inherited from the mother’s father, the reality is that the genetic component of MPB is not fully understood and is believed to be polygenic, involving multiple genes.
Introduction:
Humans have 23 pairs of chromosomes that carry their genetic information, including traits like eye color and toe length. Among these pairs, the “X” and “Y” chromosomes determine biological sex, with women having two “X” chromosomes and men having one “X” and one “Y” chromosome. The gene associated with baldness, called the AR gene, is found on the “X” chromosome. A study of 12,806 men of European ancestry revealed that those with the AR gene had more than twice the risk of developing MPB compared to those without it.
However, the AR gene is not the sole determinant of baldness. Further research in a 2017 review identified 63 genes that may play a role in male pattern baldness, with only six of them found on the “X” chromosome. Additionally, studies have shown that more than 80 percent of individuals experiencing noticeable balding had a father who also experienced hair loss.
A Closer Look at DHT:
Dihydrotestosterone (DHT) is a by-product of testosterone, formed through the action of the enzyme Type I and II 5-alpha-reductase, which is present in the oil glands of the hair follicles. While the genetic process of male pattern baldness is now better understood, scientists have known for over three decades that DHT plays a key role in shrinking hair follicles through a process known as miniaturization.
Miniaturization is a biological process driven by hormones that results in the shrinking of hair follicles over time, eventually leading to a bald scalp. The hair follicle growth cycle consists of three phases: the growth phase (anagen), the transitional phase (catagen), and the resting phase (telogen). In hair follicles that are genetically susceptible, the hormone dihydrotestosterone (DHT) can cause the growth phase of the hair cycle to become progressively shorter. As a result, the individual hairs produced by these follicles are unable to reach their full size due to the shortened growth window. Over time, these hairs decrease in size, including both diameter and length, until they eventually disappear. This process of miniaturization is the primary mechanism underlying androgenetic alopecia, also known as genetic hair loss /Male Pattern Baldness.
However, with proper intervention, the miniaturization process can be slowed down or even stopped if detected early enough. Today, there are interventions available that can help in managing the effects of DHT on hair follicles and potentially prevent further hair loss. Early detection and intervention can be crucial in managing the impact of DHT on hair follicles and maintaining healthy hair growth.











 Diagnosis:
Diagnosis: